MIPS Value Pathways (MVPs)
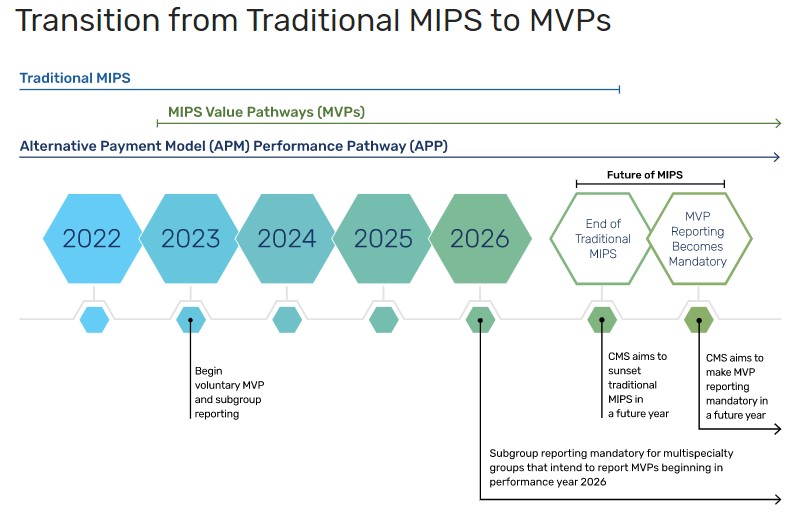
MIPS Value Pathways (MVPs) is an additional Medicare Quality Payment Program (QPP) participation track that came available in 2023, and offers a reporting option aside from the Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APMs). This option is meant to reduce reporting burden, encourage meaningful participation, and improve patient outcomes. MVPs are an optional way to meet MIPS reporting requirements beginning with the 2023 performance year.
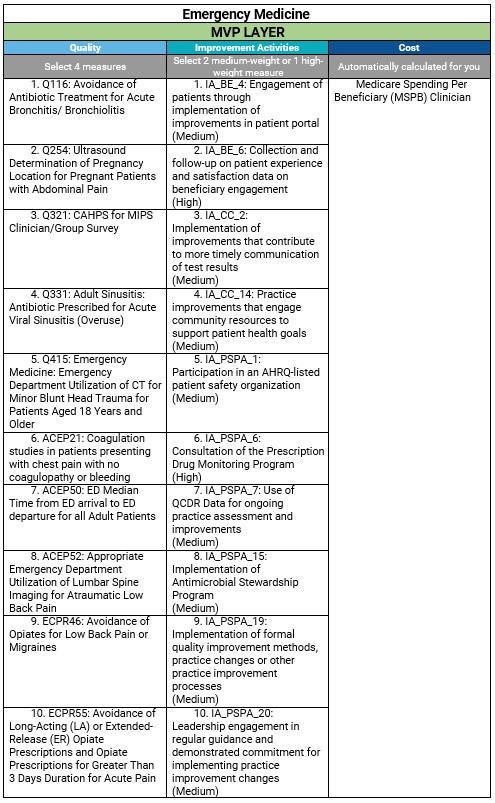
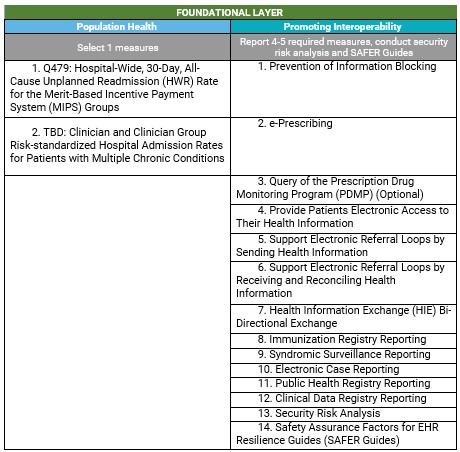
MIPS Value Pathways (MVPs) are designed to align measures and activities from the four MIPS performance categories. The new framework is intended to allow MVP participants to report on a smaller subset of measures and activities (within the measures and activities available for traditional MIPS) that are
relevant to a specialty, clinical condition, patient population, or episode of care and are more meaningful to a clinician's practice, specialty, or public health priority. Reporting requirements include the same four performance categories that MIPS has always included, plus a foundational layer of promoting interoperability and population health measures. New measures and activities will be proposed through future rulemaking and finalized via the annual Physician Fee Schedule. The timeline for sunsetting traditional MIPS has not been finalized, but MVP reporting will become mandatory at some point in the future.
Finalized MVPs Policy:
The finalized policies, measures, and activities for each year are published in the annual Physician Fee Schedule and on the
CMS QPP website (select the appropriate year). On the website, select the year and medical specialty to find the MVPs available for reporting for that year.
Who Can Report:
- Individual clinicians - Select this option to register a single clinician to report an MVP. You can register to report an MVP as an individual in addition to reporting an MVP as part of a group
- Group - Select this option to register to report one MVP as a group, on behalf of all the clinicians in your practice. You can register as a group in addition to registering individual clinicians or a subset of clinicians to report a different MVP. Starting in 2026, multispecialty groups (that aren’t small practices) intending to report MVPs will be required to report as subgroups or individuals.
- Subgroups - Select this option to register a subset - some but not all - of the clinicians within your practice to report one MVP as a subgroup. Recommended for multispecialty groups to allow for reporting of more than one MVP based on clinical relevance. Subgroup participation will be required for multispecialty practices wishing to report MVPs beginning in the 2026 performance year. Starting in 2026, multispecialty groups (that aren’t small practices) intending to report MVPs will be required to report as subgroups or individuals.
- APM entity - Select this option to register as an APM Entity to report an MVP.
Reporting Requirements:
- Quality - Accounts for 30% of the final score. Participants will select four quality measures available, including one outcome measure (or a high priority measure if an outcome is not available or applicable) and collect and submit data for the 12-month performance period (January 1 – December 31). Performance data will need to be reported for at least 75% of the denominator-eligible cases for each measure.
- Improvement Activities (IA) - Accounts for 15% of the final score. CMS removed the activity weightings and simplified requirements by reducing the number of activities clinicians are required to attest to completing. For MVP reporting, clinicians, groups, and subgroups (regardless of special status) must attest to 1 activity in a continuous 90-day performance period (during calendar year 2026) unless otherwise stated in the activity description. Clinicians may still choose to report a Patient-Centered Medical Home (PCMH) improvement activity if participating in a PCMH.
- Cost - Accounts for 30% of the final score. Participants' performance will be calculated exclusively on the cost measures included in the MVP using administrative claims data.
- Foundational Layer (MVP Agnostic) - Accounts for 25% of the final score. Data is to be collected for a minimum of 180 continuous days during the calendar year. The foundational layer has 2 components:
- Promoting Interoperability (PI) - Participants will report on the same PI measures required under traditional MIPS unless they qualified for automatic reweighting or had an approved hardship exception.
- Population Health Measures - CMS will calculate these measures through administrative claims and will be scored as part of the quality performance category.
Scoring:
Participants will receive a final score based on the same performance category weights used in traditional MIPS, and the same performance category weight redistribution policies apply. Review our
MIPS Step-By-Step Guide for scoring and weighting. Beginning with the 2026 performance period, there will be a 2-year informational-only feedback period for new cost measures, where clinicians will receive feedback on new measures, without these measures impacting their scores. Clinicians won’t receive any informational-only feedback for the 2026 performance period because no new cost measures were added to the program. Clinicians can earn up to 1 percentage point (out of 100) for cost improvement.
Small Practices:
Small practices continue to have flexibilities when reporting an MVP, just as in traditional MIPS:
- They’ll meet quality reporting requirements by reporting all Medicare Part B claims measures in the MVP selected, even if there are fewer than 4 measures included.
- They’ll receive 6 bonus points in the quality performance category as long as 1 quality measure is submitted, just as in traditional MIPS.
- They’ll receive 3 points for quality measures without a benchmark or that don't meet case minimum requirements, just as in traditional MIPS.
- The Promoting Interoperability performance category will be automatically reweighted when reporting an MVP(s), just as in traditional MIPS.
Small practices don’t have reduced reporting requirements in the improvement activities performance category when reporting an MVP. Beginning in 2025, all MVP participants, including small practices, must perform 1 improvement activity from those available within their selected MVP.
MVP Registration:
To register to report an MVP, sign in to the QPP website with your Health Care Quality Information System (HCQIS) Access Roles and Profile system (HARP) account. The 2025 MVP Registration Guide will be available in April and will provide detailed steps on how to complete the registration process and answer frequently asked questions.
-
You can only register for an MVP during the MVP Registration Window.
- If reporting Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS Survey as a measure in your selected MVP, you’ll need to complete both your MVP and CAHPS for MIPS Survey registrations.
- Changes to the registration cannot be made after the registration deadline, and reporting may not be submitted for any MVPs for which the participant did not register.
- You do not have to report an MVP even if registered and may instead report via traditional MIPS.
Example: Emergency Medicine MVP: