Medicaid and CHIP
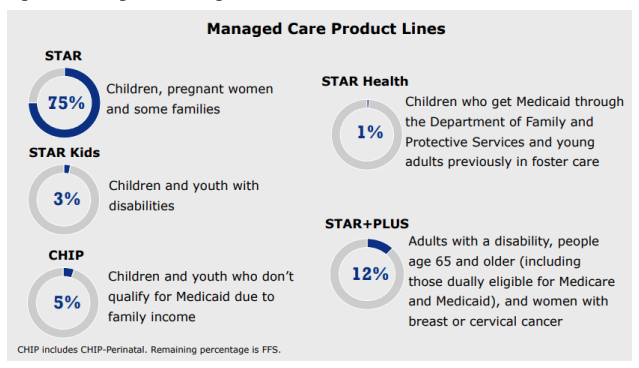
Medicaid and CHIP are programs that provide medical coverage to eligible needy people in Texas. Medicaid is a State (TMHP) and Federal cooperative venture for those who might otherwise go without medical care for themselves and their children. Most Medicaid in Texas is administered through Medicaid Managed Care Organizations (MCO) under contract with the state. Currently, there are four such programs in Texas: STAR, STAR+PLUS, STAR Health, and STAR Kids that, for the most part, offer services through MCOs. These plans often offer additional services not covered by traditional Medicaid (dental, vision, etc.).
The Children's Health Insurance Program (CHIP) offers low-cost health coverage for children from birth through age 18. CHIP is designed for families who earn too much money to qualify for Medicaid but cannot afford to buy private health coverage. Like the above programs, these services are all administered by private MCOs with their own network of providers.
More information on these programs can be found in the HHS reference guide. If unable to locate a Provider Relations representative reference HHS MCO Provider Relations Contacts.
Medicaid Managed Care Contracting and Credentialing
Physicians wishing to newly contract with MCOs now have a more streamlined process to do so through the Consolidated Verification Organization Initiative. A statewide initiative has been implemented that will allow physicians to credential through Aperture, a Credentialing Verification Organization (CVO), for all Medicaid MCOs in Texas. This process will eliminate the need to go through separate credentialing for each MCO with which you wish to contract. Once Aperture has your credentialing file, it can be used to contract with all MCOs.
The Enrollment Process:
- Enroll with TMHP if you have not already done so. Physicians must complete the enrollment process through TMHP/HHSC prior to credentialing with MCOs.
- Contact the MCOs you wish to contract with (you do not need to submit a credentialing application at this point).
- The MCOs will notify Aperture that you wish to contract and Aperture will contact you to begin the credentialing process.
- Aperture will provide you with an e-credentialing application and instructions to submit to Aperture. CAQH ProView information will be accepted. A paper application can also be accepted that will be provided to you.
- Aperture will collect your application and other required documentation (license, DEA, etc.) from you and verify the information provided. However, there may be some information that you will need to provide directly to the MCOs.
- This credentialing process is separate from the contracting process. Physicians will still need to engage with the MCO to complete the contracting process.
Expedited Credentialing:
Expedited credentialing allows providers to serve Medicaid recipients on a provisional basis while their credentialing application is pending. You must be a member of an established health care provider group who has an existing group contract in force with the MCO. For Medicaid reimbursement purposes only, once the applicant provider submits the required information, the MCO treats the provider as if they were in the MCO’s network when they provide services to a patient. If the provider qualifies for expedited credentialing, MCOs will process claims within 30 calendar days after receipt of a completed credentialing application, even if the MCO has not yet finished its review of the provider’s credentialing application.
Revalidation
Most providers must revalidate their enrollment with HHSC every three to five years, depending on provider type. Providers who are actively enrolled and are eligible to revalidate can complete a revalidation application using the TMHP Provider Enrollment Revalidation in PEMS tool. TMHP will notify providers of their revalidation deadline 180 days before the deadline. This 180-day window is the only time revalidation can be completed for each revalidation cycle. Since it usually takes about 60 days for an application to process from beginning to end (depending on how complete and accurate the application is upon submittal), it is highly recommended that providers begin the revalidation process immediately and check status on the application often to avoid disenrollment and claim denials. Once the provider submits their revalidation application, TMHP reviews it for completeness. If any omissions or deficiencies are found, TMHP will notify the provider. If deficiencies or omissions are found, the process could take longer exceeding the deadline resulting in disenrollment. Providers who have been disenrolled are not eligible for revalidation and must complete a reenrollment application instead. For instructions, visit the PEMS Step-by-Step Guide.
QMB/Dual Eligible Demonstration Project
The Dual Eligible project is a Medicaid program that helps very low-income dual eligible beneficiaries with Medicare cost-sharing. Dual eligible or QMB (Qualified Medicare Beneficiary) are terms used to identify Medicare beneficiaries who also receive Medicaid assistance, ranging from beneficiaries who receive the full range of Medicaid benefits to beneficiaries who receive assistance only with Medicare premiums or cost sharing. Dual eligible coverage is dependent on beneficiaries’ incomes and assets thresholds determined by the state. The dual eligible categories are outlined in these resources: Dually Eligible Individuals, Beneficiaries Dually Eligible for Medicare & Medicaid, and List and Definition of Dual Eligibles. More information regarding the QMB program can be found in the FAQs.
QMB beneficiaries may obtain benefits in various ways:
- By enrolling with traditional Medicare Parts A and B, and enrolling in a MCO. An example would be a patient who presents with a traditional Medicare card and a MCO card. You will bill Medicare first and Medicare will cross-over the claim to the MCO.
- By enrolling in a Medicare Advantage plan (MAP) that is designed for dual eligibles and enrolling in a MCO plan. The MAP and MCO plans may be administered by the same insurance company (e.g. UnitedHealthcare AARP and UnitedHealthcare Community Plan), or separate insurance companies (e.g. UnitedHealthcare AARP and Community Health Choice). If the patient is enrolled in plans administered by the same insurance company, the MAP may or may not cross-over the claim to the MCO so verify such before billing the MCO. If the MAP and MCO are different insurance companies, the MAP will not cross-over the claim to the MCO.
- By enrolling in a Medicare-Medicaid plan (MMP). An MMP is an alignment initiative in which Medicare and Medicaid benefits are offered as a single plan that blend a QMB's Medicare and Medicaid benefits into one plan. Physicians need only bill this one plan to receive full payment for both the Medicare and Medicaid benefits.
Federal law protects QMB beneficiaries from any cost-sharing liability and prohibits all original Medicare and Medicare Advantage providers, including those who do not accept Medicaid, from billing QMB beneficiaries for Medicare deductibles, coinsurance, or co-payments. All Medicare and Medicaid payments that physicians receive for furnishing services to a QMB beneficiary are considered payment in full. For additional information, see the
MLN Matters notice and
MLN Booklet.
Self-pay/Private Pay
Per the
Texas Administrative Code, Medicaid participating physicians must accept Medicaid payment as the full and complete payment and may not charge or take other recourse against a Medicaid patient for a service for which payment is made or will be made, except as outlined below.
Non-covered Services:
A participating physician may charge a Medicaid patient for services that are not medically necessary, or are outside the amount, duration, and scope of the Texas Medicaid Program, or are not a benefit of the Program only if:
(1) the specific service is requested by the patient; and
(2) the physician has obtained and kept a written acknowledgment, signed by the patient, that states: "
I understand that, in the opinion of (provider's name), the services or items that I have requested to be provided to me on (dates of service) may not be covered under the Texas Medicaid Program as being reasonable and medically necessary for my care. I understand that the Texas Health and Human Services Commission or its designee determines the medical necessity of the services or items that I request and receive. I also understand that I am responsible for payment of the services or items I request and receive if these services or items are determined not to be reasonable and medically necessary for my care."
Non-participating Physicians:
For a physician who does not participate in the Texas Medicaid Program, before providing a service to a Medicaid patient, the physician should inform the patient that no claim will be filed and the patient will be directly responsible for payment. It is advisable to have the patient sign an acknowledgement that they understand they will be responsible for all charges. The
TMHP Private Pay Agreement could be revised with the appropriate language to serve this purpose.
Private Pay Patients:
Per the
TMHP Provider Manual (see Client Acknowledgment Statement section), for Medicaid patients who do not want a claim submitted to Medicaid, the physician must advise the patient that they are being accepted as a private pay patient at the time the service is provided and will be responsible for paying for all services received. The patient must sign an acknowledgment statement, such as the
TMHP Private Pay Agreement, to demonstrate the patient was properly notified of private pay status.
Prior Authorization for Drugs
Managed Medicaid Plan Quicklinks
Community Health Choice (STAR, STAR+Plus, CHIP)
Molina (STAR, STAR+Plus, CHIP, MMP)
Superior Healthplan (STAR Health)
Texas Children’s Health Plan (STAR, STAR Kids, CHIP)
TMHP
UnitedHealthcare Community Plan (STAR, STAR+Plus, STAR Kids, CHIP, MMP)
Wellpoint (Amerigroup) (STAR, STAR Kids, CHIP)
Where to file complaints for STAR, STAR+PLUS, STAR Health, STAR Kids, and CHIP Medicaid Managed Care Plans:
Physicians must exhaust the complaint or grievance process with the Medicaid managed care plan before
filing a complaint with HHSC. If after doing so the provider believes they did not receive full due process from the plan, they may file a complaint at
HPM_complaints@hhsc.state.tx.us, via the
online complaint portal, or in writing at the address below. The complaint process can be found on the
HHS flow chart.
Texas Health and Human Services Commission
Medicaid/CHIP
Health Plan Management
Mail Code H-320
P.O. Box 85200
4900 N. Lamar
Austin, TX 78708-5200
Resources: