IMPLEMENTING TELEMEDICINE IN YOUR PRACTICE
If your organization is considering implementing a telemedicine program but you currently have limited experience with telemedicine systems, please review the following information to assist you and your practice in this process.
Contract Language:
Contracts are a necessary part of any telemedicine venture. A telemedicine service contract will share many of the same contracting concerns as an EHR, such as who owns the equipment, who owns the data, and expectations around service call timing, up-time, software updates and turnaround times. Agreements made with telemedicine providers or technology vendors should be reviewed to ensure that insurance provisions include mutual hold-harmless and indemnification language and that adequate insurance coverage is required. Confer with legal counsel to determine which state laws apply to the organization’s telemedicine services, monitor changes in applicable regulations and take steps to ensure that procedures for education and compliance are in place. The American Society for Health Care Risk Management has developed a white paper discussing Telemedicine Risk Management Considerations.
The Coker Group offers TMA/HCMS physician members free technology contract review services. Coker Group is a member of TMA-approved Group Discount Programs.
Policy and Procedures:
Although telemedicine has the potential to improve several aspects of medical care, such as facilitating physician-patient communication and monitoring treatment of chronic conditions, telemedicine poses unique challenges in ensuring patient-safety and privacy of health information. Therefore, it is prudent for telemedicine providers to develop a comprehensive set of policies and procedures (P&P). The TMA has developed templates to assist practices in developing their own P&P. These can be found under the section titled “Policies, Procedures and Forms for Telemedicine Services” on their own P&P. These can be found under the section titled “Policies, Procedures and Forms for Telemedicine Services” on their
Telemedicine in Texas web page.
Additionally, organizations considering telemedicine or adding new telemedicine technologies to an already existing panel of services must consider how the new or added services will be incorporated into privacy and security policies, procedures, and workflows. For example:
- Incorporate telemedicine into the Notice of Privacy Practices.
- Include telemedicine equipment in the organization’s Security Management Plan and annual Security Risk Assessment.
- Ensure all staff and providers who participate in telemedicine services have received telemedicine specific healthcare privacy and security training.
- Determine the need for Business Associate Agreements. Evaluate all parties, including any vendors involved in the provision of services, for compliance with federal and state privacy and confidentiality regulations, and require the ability to provide proof compliance if asked. Require telemedicine vendors to hold their subcontractors accountable as well.
Vendors:
Below are resources to help identify a vendors and resources for telemedicine implementation:
Educational Resources/Webinars:
RULES AND LEGISLATION
Texas Requirements
For the current TMB telemedicine rules, please review the
Texas Administrative Code. Additional information is available on the TMA General Counsel's white paper "
Texas Laws and Regulations Relating to Telemedicine". For audio-only telemedicine in Texas, review the has specific
requirements before providing these services as they may be more stringent than those found in HIPAA.
Out-of-State licensure requirements
A number of states have passed legislation to permanently allow out-of-state physicians to practice telehealth in their state if they follow the state’s requirements. Some states allow out-of-state physicians and other providers to practice telehealth in their state if they are already licensed in another state. Other states require out-of-state telehealth license recipients to pass an exam. You’ll need to refer to state licensing boards to determine if that state offers a telehealth registration option, and if so, what are the requirements. Details can be found at
HHS.
PAYOR POLICIES
Commercial
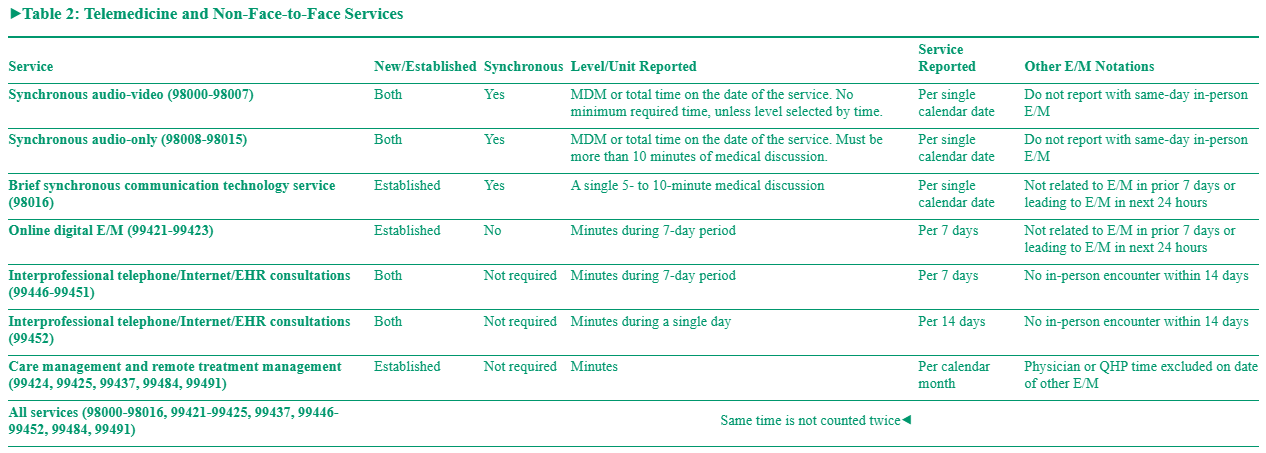
In general, most Texas telemedicine legislation applies only to fully-insured plans (TDI or DOI on front of patients insurance card), thus coverage for telemedicine varies by plan and the patient's benefits. The Telemedicine Billing and Coding Quick Reference Chart by Payer provides information by payor. However, coverage, benefits, and coding requirements should be verified prior to rendering telemedicine services. in 2025, CPT developed a set of telemedicine codes to replace the E/M codes for billing virtual services (Medicare does not recognize these new codes). Refer to the CPT manual for coding guidance.
Medicare
Medicare covers various telemedicine services, each with their own stipulations and requirements. Consult the MLN Fact Sheet for a list of services, billing guidance, etc. and the Telehealth Services web page. More information is available at Telehealth.HHS.gov. Visit the Center for Connected Health Policy's Billing for Telehealth Encounters: An Introductory Guide on Fee-for-Service for in-depth guidance, and the Telemedicine in Texas web page for billing and coding information and other resources applicable to Texas.
Medicare’s 2025 telemedicine coding policies differ from those in the 2025 CPT book where 17 new telemedicine codes (98000–98016) were introduced. Medicare has chosen not to recognize 16 of these new telemedicine codes (98000–98015). Medicare has indicated that it has other codes that represent those services making it unnecessary to cover both sets of codes. Instead, physicians will continue to bill the standard office E/M codes (99202–99215) along with the appropriate modifier (95 for audio-visual, or 93 for audio-only) and place of service (02 for telehealth provided other than in patient’s home, or 10 telehealth provided in patient’s home). However, Medicare will recognize the new brief virtual check-in CPT code 98016, which replaces HCPCS code G2012, set to be deleted. Also, for 2025, CPT codes 99441-99443 have been deleted.
Additionally, Medicare will allow the use of audio-only telemedicine provided to a patient but only if the physician has available an audio-video telecommunications system but the patient is unable or does not consent to use video. As codes 99441-99443 are no longer available, bill these visits with codes 99202-99215 with modifier 93, and POS 02 or 10. CMS has also stated the following elements will be necessary when billing for audio-only services:
• Documentation must reflect that the physician has audio-video available, but the patient preferred audio-only or was unable to use audio-video; and
• Modifier 93 must be appended to services provided via audio-only (for RHCs and FQHCs, modifier FQ).
There are 4 types of Medicare virtual services available to Medicare beneficiaries:
1. Telehealth/Telemedicine Visits: Telemedicine is the use of electronic information and telecommunications technologies to provide care. Technologies for telehealth include videoconferencing, store-and-forward imaging, streaming media, and terrestrial and wireless communications. Beginning Jan. 1, 2024, bill POS 02-Telehealth to indicate telemedicine services were provided to a patient in an originating site other than the patient’s home. Bill POS 10-Telehealth for services provided to patients in their home.
2. Virtual Check-Ins: Virtual check-ins are brief phone calls or video chats to see whether patients need to have an in-person visit. New and established patients in all geographical locations may receive this service from their homes and have a brief communication with physicians using various applications including telephones, or exchange information through video or images. The communication cannot be related to a medical visit within the previous seven days and may not lead to a medical visit within the next 24 hours (or soonest appointment available). The patient must verbally consent to receive virtual check-in services.
3. E-Visits: E-visits are non-face-to-face patient-initiated communications through an online patient portal. Available in all locations, including the patient’s home, and all geographical areas, for established patients only. Medicare patients may have non-face-to-face patient-initiated communications with their physicians using online patient portals. Patients must generate the initial inquiry, and communications can occur over a seven-day period. The services may be billed using CPT codes 99421-99423 and HCPCS codes G2061-G2063, as applicable.
4. Telephone (audio-only): Audio-only services are only permissible if the physician has an audio-video telecommunications system but the patient is unable, or does not consent, to use video. The patient must be receiving the service from home. However, the patient’s home is a permissible originating site only for services for the diagnosis, evaluation, or treatment of a mental health or substance use disorder, and for the monthly ESRD-related clinical assessments.
Medicare Advantage
Medicare Advantage plans are required to cover all Part A and Part B benefits covered under traditional Medicare. Medicare Advantage plans also have the flexibility to offer additional telemedicine benefits not routinely covered by traditional Medicare. Telemedicine benefits should be verified prior to rendering services for each patient to ascertain coverage, reimbursement, and coding requirements.
Medicaid
Consult the current
provider manual under the Telecommunication Services Handbook for Texas Medicaid fee-for-service benefits. Also consult the TMHP
COVID-19 page for updates (see the
Recent News column on the right side of the page for specific notices) that may provide current flexibilities beyond the information in the provider manual. For information about managed care benefits please contact the patient's plan. Medicaid, Medicaid managed care organizations (MCOs), and the Healthy Texas Women Program continuously update their coverage polices. Texas Medicaid managed care organizations must provide all medically necessary, Medicaid-covered services to eligible clients. Administrative procedures such as prior authorization, pre-certification, referrals, and claims filing may differ from traditional Medicaid and from MCO to MCO. Providers should contact the client's specific plan for coverage and billing guidance.
**The information provided on this page is subject to change and should be verified independently.**