2024 MIPS Step-by-Step Guide
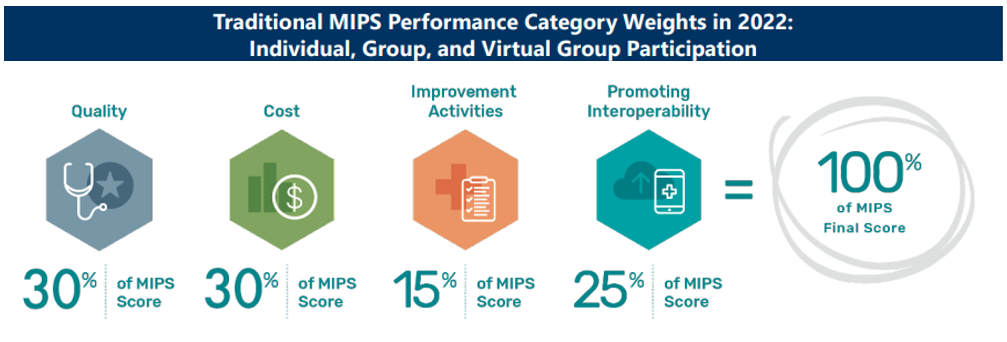
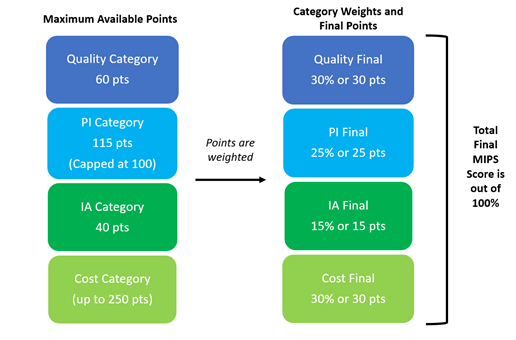
This guide provides a high-level overview and examples of calculations for the Merit-Based Incentive Payment System (MIPS) performance categories of Quality (30 final MIPS points), Promoting Interoperability (25 final MIPS points), Improvement Activities (15 final MIPS points), and Cost (30 final MIPS points). The Cost category does not require data submission and is scored through claims submitted to Medicare. Below are details on calculating, collecting, and reporting each MIPS performance category with links to additional information. Calculating performance category points will vary on the participation level and collection type chosen by the physician. Also, Special Status is automatically assigned by CMS and may affect your reporting requirements. Small practices have Special Status and are eligible for special considerations. For more specific details, visit QPP’s Resource Library.
 `
`
A maximum of 100 final MIPS score can be earned by achieving the full points in each category.
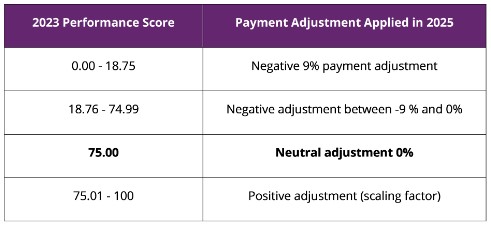
Using a composite performance score, eligible clinicians (ECs) may receive a payment bonus, a payment penalty or no payment adjustment. Eligible Clinicians (EC) will need to earn enough points in each category to achieve a total MIPS score greater than or equal to 75 points to avoid a 9% payment reduction/penalty in their 2026bo Part B reimbursements. Any MIPS score over 75 points could result in incentive payment by increasing their 2025 Part B reimbursements. The percentage increase available is dependent on several scaling factors (not to exceed 3.0) to ensure that the adjustments are budget neutral. For more information about the MIPS program and steps on getting started please review our MIPS page.
2023 PY and 2025 Payment Adjustments
Quality Step-by-Step Guide (be sure to select current year, then click on the Guide's link at bottom of page)
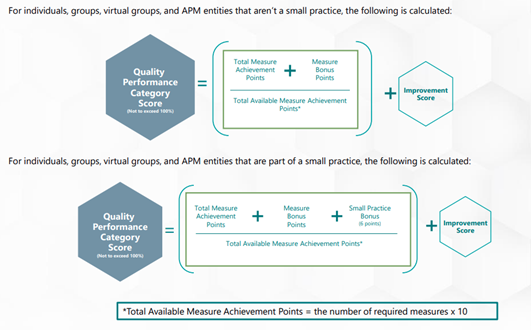
The Quality category accounts for 30 final MIPS points out of the possible 100 final MIPS score. This category requires data reporting for a full calendar year on at least 6 selected measures. To achieve data completeness, you must identify the eligible population (denominator)
as outlined in the measure’s specification and must report performance data (met or not met, numerator exclusions, or denominator exceptions) for at least 75% of the eligible population (excluding denominator exclusions).
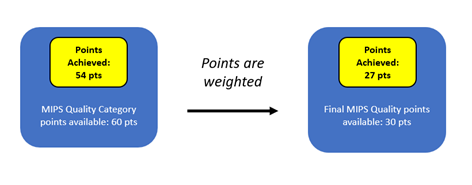
Each measure is worth up to 10 points (allowing for a maximum of 60 available points), and depending on performance physicians/practices will receive between 0 and 10 points per measure. Up to 10 additional percentage points are available based on a physicians’ improvement in their quality performance category from the previous year. If CMS can’t compare data between 2 performance periods, or there is no improvement, the improvement score will be 0%. The improvement score can’t be negative. Additonally, for small practices 6 bonus points will continue to be added to the quality performance category score for clinicians in small practices who submit at least one measure.
Example (does not consider any possible bonus points or improvement scoring practices could achieve such as the small practice bonus and others offered within MIPS):
Dr. Smith reported on 6 quality measures. On three of her measures, she received the full 10 measure points, but on the other three she was only able to achieve 8 measure points each. Since three of the measures submitted were new measures for the performance year, they will earn 7-10 points if a performance benchmark can be created, and data completeness and case minimum criteria is met.
(10 points x 3 measures) + (8 points x 3 measures) = 54 category points
54 category points ÷ 60 category measure points possible = .90 or 90%
Because Dr. Smith achieved 90% of her category measure points, she can apply 90% of the 30 final MIPS Quality points available to her final MIPS score:
30 final MIPS Quality points x .90 or 90% = 27 final MIPS points
Dr. Smith’s FINAL MIPS Quality score is 27 points, which will be counted towards her final MIPS score. This point total is less than the 75 MIPS points benchmark, therefore Dr. Smith will have to participate in other categories to potentially receive an incentive payment for achieving > 75 MIPS points, or to avoid a penalty in the subsequent payment year.
The PI category accounts for 25 final MIPS points out of the possible 100 final MIPS score. This category now requires a performance period of at least 180 consecutive days in the performance year. Total available category points are 115 with a capped category score of 100 possible measure points (no less than 100 points in the denominator when scored).
For 2024, the PI category requires the use an Electronic Health Record (EHR) that meets the certification criteria at 45 CFR 170.315 for participation in this performance category to align with the Office of the National Coordinator for Health Information Technology (ONC)’s current and future regulation. Participants must submit collected data for certain required measures (5 to 6 required measures) from each of the 4 objectives measures (unless an exclusion is claimed).
In addition to submitting measures, clinicians must provide their EHR’s CMS Identification Code from the Certified Health IT Product List (CHPL) and submit a ”yes” to:
- The Prevention of Information Blocking Attestation,
- The ONC Direct Review Attestation,
- The security risk analysis measure, and;
- The SAGER Guides measure
You can earn 5 bonus points for submitting a “yes” response for one of the optional Public Health and Clinical Data Exchange measures (Public Health Registry Reporting, Clinical Data Registry Reporting, or Syndromic Surveillance Reporting). You’ll be awarded full points if a “yes” is submitted for the 2 required measures (Immunization Registry Reporting and Electronic Case Reporting) or one “yes” and one exclusion. You’re also required to submit your level of active engagement for these 2 measures.
You will receive 0 points in the PI performance category if you fail to submit a required attestation, report nothing in the numerator on a required measure, or claim an exclusion for a required measure.
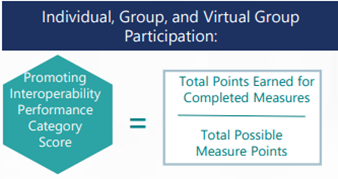
Example:
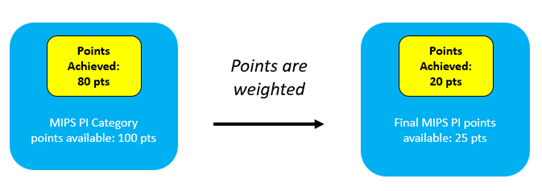
Dr. Smith’s EHR is ONC certified. After completing all the required PI measures Dr. Smith achieves 80 category points (we use 100 category points possible for this calculation rather than the total possible of 115 because this category is capped at 100 points).
80 category points ÷ 100 category points possible = .8 or 80%
Because Dr. Smith achieved 80% of her category points, she can apply 80% of the 25 final MIPS PI points available to her final MIPS score.
25 final MIPS ACI points x .80 or 80% = 20 final MIPS points
Dr. Smith’s final MIPS PI score is 20 points, which will be counted towards her final MIPS score. This point total does not meet the 75 MIPS points benchmark; therefore Dr. Smith will have to participate in other categories to potentially receive an incentive payment for achieving > 75 MIPS points, or to avoid a penalty in the subsequent payment year.
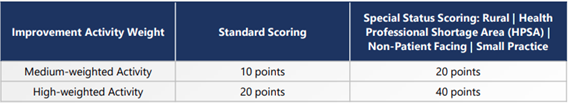
The IA category accounts for 15 final MIPS points out of the possible 100 final MIPS score. This category requires each activity selected to be implemented within your practice for at least 90 consecutive days during 2023. This category is attestation based, which means only a “yes” or “no” statement is required for each activity completed when the reporting period begins. No documentation is required to be submitted but it is important to keep record of the activity completion in case of an audit by CMS.
There are two levels of activities medium-weighted and high-weighted activities. Generally, you must complete 2 high-weighted activities (each worth 20 category points) or 4 medium-weighted activities (each worth 10 category points), or 2 medium and 1 high weighted activities. to achieve a full 40 out of 40 maximum category points. For those with Special Status, you’ll receive double points for each high- or medium-weighted activity you submit. You can check for any special status by signing in to qpp.cms.gov.
Small practices (15 clinicians or fewer) have Special Status and earn 2x the points for each improvement activity submitted when reporting traditional MIPS. They can complete 1 high-weighted activity (worth 20 category points) or 2 medium-weighted activities (each worth 10 category points), or 2 medium and 1 high weighted activities to achieve a full 40 out of 40 maximum category points, resulting in receiving the full 15 final MIPS points towards their final MIPS score.
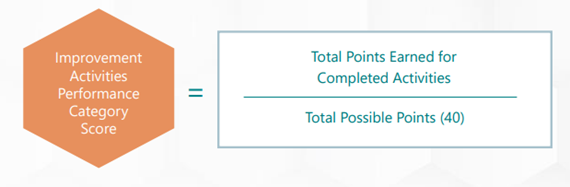
Example:
Dr. Smith (small practice Special Status) has selected 2 medium weighted activities to complete (activities completed by a practice can be attested to by an individual or group).
(1 medium activity x 20 points) + (1 medium activity x 20 points) = 40 category points
40 category points ÷ 40 category points possible = 1 or 100%
Because Dr. Smith achieved 100% of her category points, she can apply 100% of the 15 final MIPS IA points available to her final MIPS score:
15 final MIPS IA points available x 1 = 15 points
Dr. Smith’s final MIPS IA score is 15 points, which will be counted towards her final MIPS score.
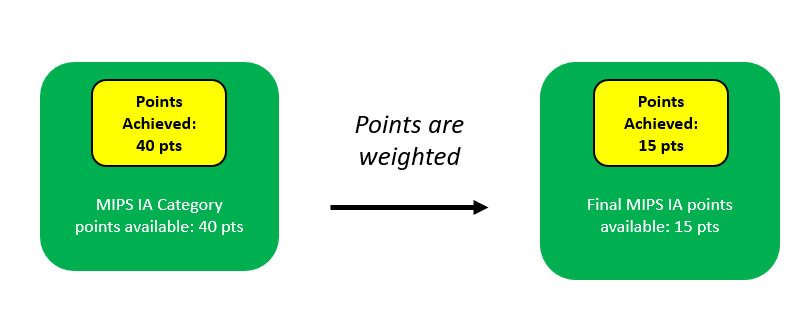
Larger practices (greater than 15 clinicians) will be required to do double the number of activities to achieve a full 40 category points (following the standard scoring) to obtain their 15 final MIPS points. They can complete 2 high-weighted activity (worth 20 category points) or 4 medium-weighted activities (each worth 10 category points), or 1 medium and 2 high weighted activities to achieve a full 40 out of 40 maximum category points, resulting in receiving the full 15 final MIPS points towards their final MIPS score.
Cost Point Calculation (be sure to select current year, then click on the Guide's link at bottom of page)
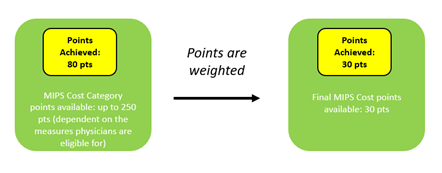
This category accounts for 30% of the MIPS final score. Claims data is used to calculate cost measure performance, which means clinicians and groups don’t have to submit any data for this performance category. Total number of category points available in the Cost category is determined by which measures apply to your practice. Measure achievement points are determined by comparing performance on a measure to a performance period benchmark. Cost measure benchmarks are calculated using performance data from the performance period, rather than historical data. If you don't meet the established case minimum for any of the available cost measures, the cost performance category will receive zero weight when calculating your final score and the 30% will be distributed to another performance category (or categories). Cost Improvement Scoring (1%) will also be calculated and apply if CMS can compare data between 2 performance periods.
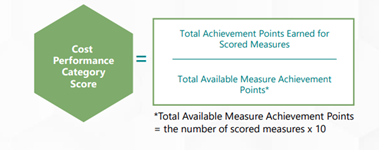
Example:
Dr. Smith was informed by CMS that she was only eligible for 8 out of the 25 available measures, therefore, she will be scored only on the measures that met the case minimum. She received 10 points on all 8 measures she was scored on.
Total Available Measure Achievement Points = (8 measures x 10 measure points)
= 80 category points possible
Total Achievement Points Earned for Scored Measures = 80 Category points scored / 80 Category points possible
= 1 or 100%
Although there are 25 total measures, Dr. Smith was only eligible for 8 measures so she will only be scored on those that she is eligible for, bringing her total max category points to 80 rather than 100.
Because Dr. Smith (and her practice) achieved 100% of her category points, she can apply 100% of the 30 final MIPS Cost points available to her final MIPS score:
30 final MIPS Cost points available x 1 = 30 points
Total points and final MIPS score for Dr. Smith
With a final MIPS score of 92 out of a possible 100, Dr. Smith will avoid a 9% penalty to her 2025 Medicare Part B payments and will most likely receive incentive payments as well.
Final MIPS Quality Score = 27
+
Final MIPS PI Score = 20
+
Final MIPS IA Score = 15
+
Final MIPS Cost Score = 30
= Total Final MIPS Score = 92