MIPS Value Pathways (MVPs)
The Centers for Medicare and Medicaid Services (CMS) introduced an additional QPP participation track, aside from the Merit-based Incentive Payment System (MIPS) and Advanced Alternative Payment Models (APMs), to reduce reporting burden, encourage meaningful participation, and improve patient outcomes.
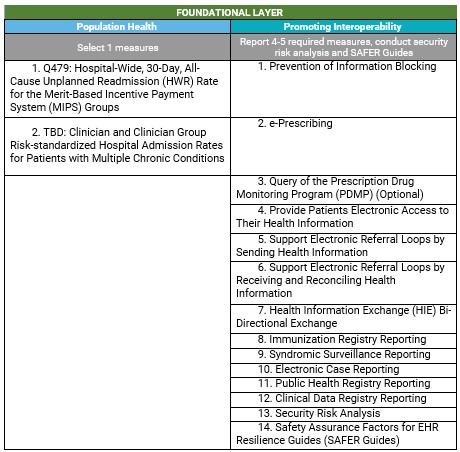
MIPS Value Pathways (MVPs) are designed to align measures and activities from the four MIPS performance categories around a specialty, medical condition, or patient population, developed by specialty societies and other AMA stakeholders. The goal is to move away from siloed reporting of measures and activities towards focused sets of measures and activities that are more meaningful to a clinician's practice, specialty, or public health priority. CMS intends to continue partnering with external stakeholders to create new MVPs so that every specialty and subspecialty has an available MVP to report. New MVPs will be proposed through future rulemaking and finalized via the annual Physician Fee Schedule. The timeline for sunsetting traditional MIPS has not been finalized, but MVP reporting will become mandatory at some point in the future.
Finalized MVPs Policy
In the 2023 Physician Fee Schedule (PFS) Final Rule, CMS finalized seven MVPs that are available beginning with the 2023 performance year as an optional reporting pathway. For implementation guidance, scoring, and other information, review the 2023 MVPs Implementation Guide.
12 MVPs for the 2023 performance year:
- Adopting Best Practices and Promoting Patient Safety within Emergency Medicine
- Advancing Cancer Care
- Advancing Care for Heart Disease
- Advancing Rheumatology Patient Care
- Coordinating Stroke Care to Promote Prevention and Cultivate Positive Outcomes
- Improving Care for Lower Extremity Joint Repair
- Optimal Care for Kidney Health
- Optimal Care for Patients with Episodic Neurological Conditions
- Optimizing Chronic Disease Management
- Patient Safety and Support of Positive Experiences with Anesthesia
- Promoting Wellness
- Supportive Care for Neurodegenerative Conditions
Who Can Report:
The below may report under a single MVP. However, beginning in the 2026 performance year, multispecialty groups will be required to form subgroups to report under an MVP. Also, voluntary reporters, opt in eligible clinicians, and virtual groups aren’t able to report an MVP for the 2023 performance year.
- Individual clinicians
- Single specialty groups
- Multispecialty groups (in 2026 multispecialty groups will be required to form subgroups)
- Subgroups
- APM entities
Reporting Requirements:
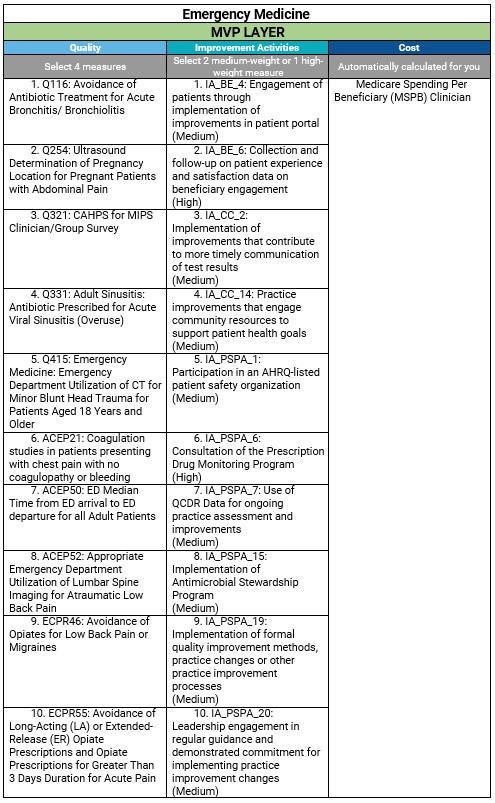
- Quality - Participants will select four quality measures available, including one outcome measure, or high-priority measure if an outcome measure is unavailable or applicable. The 4 required quality measures don’t include the required population health measures evaluated as part of the foundational layer.
- Improvement Activities - Participants will select two medium-weighted improvement activities, or one high-weighted improvement activity, or a Patient-Centered Medical Home (PCMH) improvement activity if participating in a PCMH.
- Cost - participants performance will be calculated exclusively on the cost measures that are included in the selected MVP using administrative claims data, even if additional cost measures (outside your selected MVP) are available for scoring.
- Foundation Layer (MVP Agnostic) - The foundational layer is composed of the Promoting Interoperability performance category and population health measures calculated through administrative claims. These measures and activities apply to all MVPs regardless of clinical specialty or medical condition. Performance is added to the Quality category score.
- Promoting Interoperability (PI) - Participants will report on the same PI measures required under traditional MIPS unless a Hardship Exception application has been approved for this category.
Scoring:
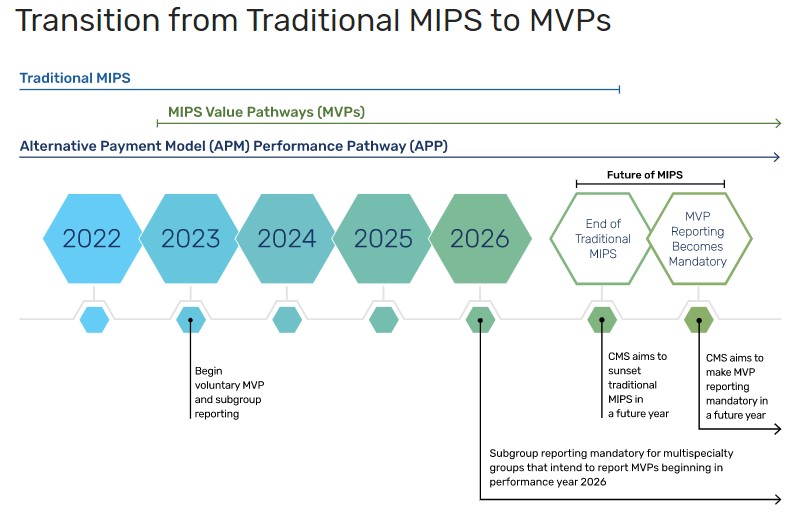
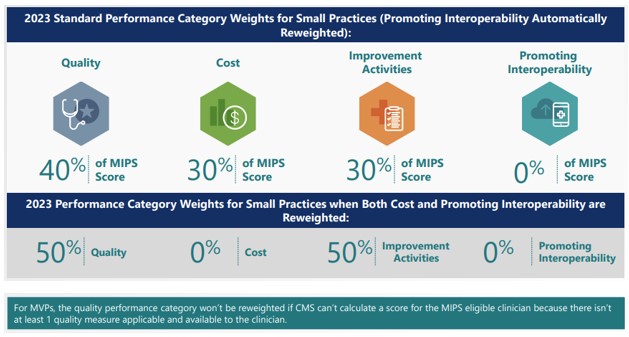
An MVP participant will receive a final score based on the same performance category weights used in traditional MIPS, and the same performance category weight redistribution policies apply.
MVP Registration Deadlines:
- MVP reporting becomes available in CY 2023. Participants and subgroups must register between April 3 and November 30 of the performance year and select the MVP they wish to report .
- If reporting Consumer Assessment of Healthcare Providers and Systems (CAHPS) for MIPS Survey associated with an MVP, a group, subgroup, or APM entity must complete their MVP registration by June 30 of the performance year.
- Participants must also select the one population health measure they intend to report, and any outcomes-based administrative claims measure on which they intend to be scored.
- Changes to the registration cannot be made after the November 30 deadline, and reporting may not be submitted for any MVPs for which the participant did not register.
- For small practices reporting through Medicare Part B claims, to meet data completeness requirements, you’ll need to start reporting the Medicare Part B claims measures in your selected MVP in January 2023, prior to the MVP registration window.
Example: Emergency Medicine MVP